Personalised support,
lasting results
Services
- Assessment
- Diagnosis
- Treatment
- Follow-up management
- Referral
- Soft tissue mobilisation
- Occupational Health
- Dry needling
- Fibreglass casting
- Thermoplastic splinting
- Joint manipulation
- Joint mobilisation
- Prehabilitation & rehabilitation exercise program & guidance
- Concussion
- Headaches / migraines
- Neck
- Shoulder
- Elbow / forearm
- Wrist / hand
- Spinal Pain (Upper, Mid, and Lower Back)
- Hip / groin
- Thigh
- Knee
- Shin / calf
- Ankle and foot

Assessment
We aim to gather all relevant information necessary to make an optimal diagnosis and develop appropriate treatment strategies, ranging from the patient’s background information to their specific concerns.

Diagnosis
Based on the assessment, we aim to make the most precise diagnosis possible while considering other potential hypotheses relevant to the patient’s specific context and the pathophysiology of their condition.

Treatment
We provide evidence-based treatment tailored to the underlying cause.

Follow-up management
We monitor the progress of the treated condition using objective outcome measures and adjust the ongoing management plan accordingly based on the results.

Referral
If progress indicates the need for further investigation, we will refer the patient to the appropriate professionals, including other allied health providers, GPs, and specialists.

Soft tissue mobilisation
Soft tissue mobilisation is a hands-on technique used to treat muscles, fascia, ligaments, and tendons, the “soft tissues” of the body. Its goals are to reduce pain, improve mobility, increase circulation, and promote healing.

Occupational Health
1. Prevention of Work-Related Injuries
Ergonomic assessments (e.g., desk setup, lifting techniques)
Education on posture, body mechanics, and injury prevention
Exercise programs to reduce risk of musculoskeletal disorders (e.g., back pain, RSI)
2. Rehabilitation for Return to Work
Physiotherapy treatment after a workplace injury
Gradual return-to-work plans
Exercise programs to reduce risk of musculoskeletal disorders (e.g., back pain, RSI)
3. Workplace Health Promotion
Wellness programs (stretching at work, physical activity, etc.)
Stress management and mental well-being strategies
Advice on reducing sedentary behavior
4. Fit-for-Work Assessments & Job-Specific Training
Assessing whether a worker can meet the physical demands of a role
Tailored training to build strength, mobility, or endurance for specific job tasks

Dry needling
Myofascial pain syndrome
Muscle tightness or spasms
Chronic pain conditions (like neck pain, back pain, shoulder pain)
Sports injuries
Tendonitis
Joint dysfunction

Fibreglass casting
Fractures (broken bones): arm, leg, wrist, ankle, etc.
Severe sprains
Post-operative support
Correction of deformities in children (e.g., clubfoot)

Thermoplastic splinting
Post-surgical joint protection (e.g., tendon repairs)
Fracture bracing (non-weight-bearing)
Nerve injuries (e.g., radial/ulnar nerve palsy)
Joint deformity correction (e.g., rheumatoid arthritis)
Burn or scar contracture prevention
Spasticity control in neurological conditions (e.g., stroke, cerebral palsy)

Joint manipulation
Releasing joint restrictions
Reducing pain quickly
Restoring lost motion
Improving alignment or biomechanics

Joint mobilisation
Pain reduction
Improving joint stiffness
Increasing range of motion (ROM)
Enhancing joint nutrition (synovial fluid movement)

Prehabilitation & rehabilitation exercise program & guidance
1. Prehabilitation
Prehabilitation is a preventive physiotherapy program designed to enhance strength, flexibility, cardiovascular fitness, and neuromuscular control before surgery or in high-risk individuals (e.g., athletes, elderly, people with chronic conditions).
2. Rehabilitation
Rehabilitation is the structured process of restoring function and reducing disability after injury, surgery, or illness through individualised physiotherapy programs.
3. Goals of Rehabilitation
Restore strength, range, endurance
Control pain and swelling
Improve joint mobility
Prevent complications (e.g., contractures, atrophy)
Return to work, sport, or daily activities
Telehealth consultations available upon request

Concussion
1. What It Is & Common Types
A concussion is a mild traumatic brain injury (mTBI) caused by a bump,
blow, or jolt to the head, or a hit to the body that causes the head and brain to move
rapidly back and forth. This sudden movement can cause the brain to bounce or twist inside
the skull, stretching and damaging brain cells and creating chemical changes in the brain.
Concussions are not always associated with loss of consciousness; in fact, most occur
without it.
Common types of concussions and related issues include
Sport-Related Concussion
Concussions that occur during athletic activities, often from direct impacts, falls, or
collisions in contact sports like rugby, football, hockey, or from falls in cycling,
skiing, etc.
Post-Traumatic Headache
Headaches that develop after a concussion, which can be persistent and mimic tension
headaches or migraines.
Post-Concussion Syndrome
When concussion symptoms persist for weeks, months, or even longer after the initial
injury. This includes ongoing headaches, dizziness, fatigue, irritability, and cognitive
difficulties.
Vestibular Concussion
Concussions primarily affecting the balance system, leading to prominent dizziness,
vertigo, unsteadiness, and nausea.
Oculomotor Concussion
Concussions primarily affecting the visual system, leading to eye strain, blurred
vision, difficulty tracking, and sensitivity to light.
2. Common Mechanism of Injury
Concussions often result from
Direct Impact to the Head
- Falls : Tripping, slipping, or falling from a height where the head strikes a surface.
- Sports Injuries : Collisions with other players, ground, or equipment; direct blows to
the head (e.g., from a ball, punch).
- Motor Vehicle Accidents : Head striking the dashboard, steering wheel, or window;
sudden acceleration-deceleration forces causing whiplash, even without direct head
impact.
- Assaults : Direct blows to the head.
Indirect Forces (Whiplash Mechanism)
A sudden, violent jerk or twist of the body that causes the head to accelerate and
decelerate rapidly, even if the head itself does not strike anything. This commonly
occurs in whiplash injuries from car accidents or violent shaking.
Blast Injuries
Exposure to explosive forces, particularly in military contexts, can cause concussions.
3. Common Symptoms
Concussion symptoms can vary widely, appear immediately or develop hours/days later, and may include
Physical Symptoms
Headache (often described as pressure or throbbing), nausea or vomiting, dizziness or
balance problems, visual problems (blurry vision, sensitivity to light, double vision),
sensitivity to noise, fatigue or low energy.
Cognitive Symptoms
Feeling "foggy" or "slowed down," difficulty thinking clearly, trouble concentrating,
memory problems (forgetting recent events or conversations).
Emotional Symptoms
Irritability, sadness, anxiety, nervousness, more emotional than usual.
Sleep Symptoms
Drowsiness, sleeping more or less than usual, trouble falling asleep.
4. How Physiotherapy Can Help with Concussion
Physiotherapy plays a crucial role in the accurate diagnosis, acute management, and comprehensive rehabilitation of concussions, aiding recovery and preventing persistent symptoms. Our approach is evidence-based, individualised, and focuses on safe, progressive return to activity. Here's how physiotherapy can help
Thorough Assessment
A detailed evaluation including neurological screening, balance testing (vestibular
system), eye movement assessment (oculomotor system), neck examination, and symptom
provocation to understand the unique presentation of your concussion and identify
contributing factors.
Personalised Management Plan
Based on your specific symptoms and assessment findings, we'll create a tailored plan
for your recovery.
Graduated Return to Activity
We guide you through a structured, stepwise progression back to daily activities,
school/work, and sport, ensuring symptoms do not worsen at each stage. This includes
- Physical Activity Progression : Gradually increasing light physical activity to
tolerance.
- Cognitive Activity Progression : Slowly reintroducing mental tasks and screen time.
Vestibular Rehabilitation
Specific exercises to reduce dizziness, vertigo, and improve balance, especially helpful
for concussions affecting the inner ear system.
Oculomotor (Vision) Therapy
Exercises to improve eye tracking, coordination, and reduce symptoms like blurred
vision, eye strain, and headaches related to visual dysfunction.
Neck Management
Often, neck injuries (like whiplash) accompany concussions. Manual therapy, soft tissue
release, and targeted exercises for the neck can reduce headache, stiffness, and
referred pain, which can be mistaken for or exacerbate concussion symptoms.
Exertion Testing & Return to Sport Protocol
For athletes, we conduct controlled exertion tests and guide them through structured
return-to-sport protocols to ensure safe participation and minimise the risk of
re-injury.
Education & Self-Management
Empowering you with knowledge about concussion recovery, symptom management strategies,
sleep hygiene, and energy conservation techniques to optimise healing and prevent
symptom exacerbation.
By providing expert guidance and specialised rehabilitation, physiotherapy aims to resolve your concussion symptoms, restore function, and help you safely return to your full quality of life.

Headaches / migraines
1. What It Is & Common Types
Headaches and migraines are distinct but often related conditions
characterised by pain in the head or face. Headaches typically involve general head pain,
while migraines are more severe, often accompanied by other symptoms. Both can significantly
impact daily life, but physiotherapy can often identify and address underlying
musculoskeletal contributions.
Common types of headaches and migraines include
Tension-Type Headache (TTH)
The most common type, characterised by mild to moderate pain that feels like a tight
band around the head, often accompanied by tightness in the neck, shoulders, and scalp.
It's frequently linked to stress, poor posture, and muscle tension.
Cervicogenic Headache (CGH)
Headaches that originate from issues in the neck, specifically the upper cervical spine
joints, muscles, or nerves. Pain usually starts in the neck or back of the head and
refers to the forehead, temples, or around the eyes. Movement or sustained neck postures
often aggravate it.
Migraine
A severe type of headache characterised by throbbing pain, usually on one side of the
head, often accompanied by nausea, vomiting, and extreme sensitivity to light
(photophobia) and sound (phonophobia). Some migraines include an "aura" (visual
disturbances) before the pain. While not purely musculoskeletal, neck tension can often
trigger or worsen a migraine attack.
Cluster Headache
A rare but extremely severe type of headache characterised by intense, piercing pain
usually around one eye or temple, often with symptoms like tearing, nasal congestion, or
drooping eyelid on the affected side. These occur in "clusters" over a period.
Medication Overuse Headache (MOH)
Chronic daily headaches that develop from the overuse of acute headache medications,
creating a cycle of pain and medication use.
2. Common Mechanism of Injury / Contributing Factors
Headaches and migraines are often triggered or exacerbated by various factors, including
Musculoskeletal Dysfunction (especially for TTH & CGH)
- Poor Posture : Prolonged forward head posture, slouching, "text neck," or improper
ergonomic setup, leading to chronic strain on neck and upper back muscles and joints.
- Muscle Tension : Tightness and trigger points in the neck, shoulder, and jaw muscles
(e.g., trapezius, sternocleidomastoid, suboccipitals).
- Joint Stiffness : Restricted movement in the upper cervical and thoracic spine joints.
- Whiplash/Neck Trauma : Past neck injuries can predispose individuals to chronic
headaches.
Stress
High levels of emotional or psychological stress leading to increased muscle tension and
altered pain perception.
Fatigue & Sleep Disturbances
Insufficient or poor-quality sleep can trigger headaches.
Dehydration
Lack of adequate fluid intake.
Dietary Triggers
Certain foods, caffeine withdrawal, or irregular meal times (more common with
migraines).
Environmental Factors
Bright lights, strong smells, loud noises (especially for migraines).
Hormonal Fluctuations
More common in women, linked to menstrual cycles or menopause (migraines).
3. Common Symptoms
Symptoms vary significantly by type but can include
Pain Location
- TTH : Band-like pressure around the head, tightness in neck/shoulders.
- CGH : Pain originating in the neck, referring to the forehead, temples, eyes.
- Migraine : Throbbing, usually unilateral (one-sided) pain.
Pain Characteristics
Aching, dull, throbbing, sharp, piercing.
Associated Symptoms (especially with Migraines)
Nausea, vomiting, extreme sensitivity to light (photophobia), sensitivity to sound
(phonophobia), visual disturbances (aura), dizziness.
Neck Symptoms
Stiffness, reduced range of motion, muscle tenderness in the neck and upper back.
Scalp Tenderness
Sensitivity of the scalp.
Fatigue & Irritability
Often accompany or follow headache episodes.
4. How Physiotherapy Can Help with Headaches / Migraines
Physiotherapy is highly effective in treating many types of headaches,
particularly Tension-Type and Cervicogenic Headaches, and can significantly reduce the
frequency and intensity of migraines by addressing musculoskeletal triggers. Our goal is to
identify the root cause of your pain and provide you with tools for long-term relief and
prevention.
Here's how physiotherapy can help
Thorough Assessment
A comprehensive examination of your neck, upper back, shoulders, posture, and jaw to
identify muscle imbalances, joint restrictions, nerve irritation, and postural
contributing factors. We'll also assess your specific headache triggers and patterns.
Manual Therapy
Hands-on techniques to
- Reduce Muscle Tension : Massage, trigger point release, and stretching for tight
muscles in the neck, shoulders, and suboccipital region.
- Improve Joint Mobility : Gentle joint mobilisations and manipulations (if appropriate)
to restore normal movement in the upper cervical and thoracic spine, reducing stiffness
and nerve irritation.
Targeted Exercise Prescription
A personalised exercise program to
- Strengthen Weak Muscles : Focusing on deep neck flexors, scapular stabilisers, and
postural muscles to improve neck stability and endurance.
- Improve Posture : Exercises and advice to correct and maintain optimal posture in
sitting, standing, and during daily activities.
- Increase Flexibility : Stretches for tight muscles in the neck, chest, and shoulders.
Ergonomic & Lifestyle Advice
Guidance on optimising your workspace, sleeping posture, and daily habits to reduce
strain on your neck and minimise headache triggers. This includes advice on stress
management and sleep hygiene.
Dry Needling / Acupuncture
Can be used to release stubborn trigger points in muscles contributing to headaches.
Education & Self-Management
Empowering you with a deep understanding of your headache type, triggers, and effective
strategies for self-treatment and prevention. This includes teaching you specific
exercises, relaxation techniques, and strategies for managing acute episodes.
By addressing the underlying physical drivers and empowering you with self-management strategies, physiotherapy aims to reduce the frequency and intensity of your headaches and migraines, improving your comfort and quality of life.

Neck
1. What It Is & Common Types
Neck is a complex and delicate structure made up of seven small vertebrae,
supported by numerous muscles, ligaments, and nerves. It's designed to support the weight of
your head (around 5 kg!), allow for extensive movement, and protect your spinal cord. Neck
pain arises when any of these structures are irritated, inflamed, or damaged.
Common
types of neck pain and related issues include
Mechanical Neck Pain
This is the most common type, often due to poor posture, muscle strain, or joint
stiffness in the neck and upper back. It's usually aggravated by certain movements or
sustained positions
Cervicogenic Headaches
Headaches that originate from problems in the neck. Pain often starts in the neck or
back of the head and refers to the front, side, or around the eye.
Whiplash
An injury to the neck caused by a sudden, forceful back-and-forth movement of the head,
typically from a car accident or fall.
It can affect muscles, ligaments,
discs, and nerves.
Radiculopathy (Pinched Nerve)
Occurs when a nerve root in the neck is irritated or compressed, often by a herniated
disc, bone spur, or narrowed spinal canal. This can cause pain, numbness, tingling, or
weakness that radiates down the arm into the hand or fingers.
Degenerative Conditions
As we age, wear and tear can occur in the neck's discs and joints (e.g., osteoarthritis,
degenerative disc disease). This can lead to stiffness, pain, and sometimes nerve
compression.
Torticollis (Wry Neck)
A condition where neck muscles contract, causing the head to twist to one side. It can
be acute (sudden onset, often from sleeping in a bad position) or chronic.
2. Common Mechanism of Injury
Neck pain often results from
Poor Posture
Prolonged periods of slouching, "text neck" (looking down at phones), or incorrect
ergonomic setup at work or home. This puts excessive strain on neck muscles and joints
over time.
Sudden Movements/Trauma
- Whiplash : As mentioned, sudden acceleration-deceleration forces, most commonly from
rear-end car collisions.
- Falls : Landing on your head, shoulder, or back can jolt the neck.
- Sports Injuries : Direct impact, falls, or sudden twisting motions in sports.
Repetitive Strain
Activities that involve repeated neck movements or sustained awkward positions (e.g.,
certain occupations, hobbies).
Sleeping Positions
Using too many pillows, a pillow that doesn't provide adequate support, or sleeping in
an awkward position can strain the neck overnight.
Stress
High stress levels can lead to increased muscle tension in the neck and shoulders,
contributing to pain.
3. Common Symptoms
Symptoms of neck pain can vary widely in intensity and type. They may include
Localised Pain
Aching, stiffness, or sharp pain in the neck itself.
Radiating Pain
Pain that travels down the arm, into the shoulder blade, or up into the head (leading to
headaches).
Stiffness and Reduced Range of Motion
Difficulty turning your head side to side, looking up or down. Often described as a
"creaky" or "stuck" feeling.
Muscle Spasm
Tight, knotted muscles in the neck, shoulders, or upper back.
Numbness, Tingling, or Weakness
If a nerve is pinched, you might experience these sensations in your arm, hand, or
fingers.
Headaches
Especially cervicogenic headaches, which originate from neck issues.
Clicking or Grinding Sounds
With neck movement, particularly if there's joint degeneration.
Difficulty Sleeping
Finding a comfortable position can be challenging.
4. How Physiotherapy Can Help with Neck Pain
Physiotherapy is highly effective in diagnosing and treating neck pain,
providing relief, and preventing recurrence. Our approach focuses on identifying the root
cause of your pain and empowering you with strategies for long-term management.
Here's
how physiotherapy can help
Thorough Assessment
We'll conduct a detailed examination of your neck, upper back, shoulders, and posture to
pinpoint the source of your pain and contributing factors. We'll also assess your
movement patterns, muscle strength, and nerve function.
Pain Relief Strategies
- Manual Therapy : Hands-on techniques such as massage, joint mobilisation, and soft
tissue release to reduce muscle tension, improve joint movement, and alleviate nerve
irritation.
- Dry Needling/Acupuncture : Can be used to release trigger points in tight muscles that
contribute to neck pain and headaches.
- Modalities : Applying heat or ice, or using electrotherapy (like TENS) to help reduce
pain and inflammation.
Restoring Movement & Strength
- Targeted Exercise Prescription : We'll design a personalised exercise program to
strengthen weak muscles (especially deep neck stabilisers), stretch tight muscles, and
improve the overall flexibility and range of motion in your neck and upper back.
- Postural Correction : Guidance on maintaining optimal posture in various activities
(sitting, standing, sleeping) to reduce strain.
Ergonomic Advice
Assessing your workspace, car setup, and even sleeping environment to suggest
modifications that support a healthy neck posture and prevent future pain.
Education & Self-Management
Empowering you with a clear understanding of your condition, common triggers, and
effective self-management techniques. This includes teaching you stretches, exercises,
and relaxation strategies you can use at home to maintain progress and prevent
re-injury.
Whiplash Rehabilitation
Specific, gentle exercises and manual therapy to restore neck movement and function
after a whiplash injury, preventing chronic pain development.
Radiculopathy Management
Strategies to decompress irritated nerves, reduce inflammation, and restore arm/hand
function, often involving specific exercises and nerve gliding techniques.
By addressing the underlying issues and providing you with the tools for self-care, physiotherapy aims to reduce your pain, restore full function, and help you return to your daily activities pain-free.

Shoulder
1. What It Is & Common Types
The shoulder is a highly mobile ball-and-socket joint, renowned for its
extensive range of motion. It comprises three main bones (humerus, scapula, clavicle) and is
stabilised by a complex network of muscles (especially the rotator cuff), ligaments, and
tendons. This intricate design allows for overhead reaching, lifting, and various arm
movements crucial for daily life and sport. Shoulder pain arises when any of these
structures become irritated, inflamed, or damaged, often due to overuse, injury, or
degeneration.
Common types of shoulder pain and related issues include
Rotator Cuff Tendinopathy/Tear
Inflammation (tendinopathy) or tears in one or more of the four rotator cuff tendons,
often caused by repetitive overhead activities, heavy lifting, or acute injury (e.g.,
fall onto an outstretched arm). Symptoms include pain with movement, weakness, and
difficulty sleeping on the affected side.
Shoulder Impingement Syndrome
Occurs when the rotator cuff tendons or bursa get "pinched" between the top of the arm
bone (humerus) and the acromion (part of the shoulder blade) during arm elevation. This
causes pain, especially when reaching overhead or out to the side.
Frozen Shoulder (Adhesive Capsulitis)
A condition characterised by significant pain and progressive stiffness in the shoulder
joint, leading to a severe restriction in range of motion. It typically progresses
through painful, stiffening, and thawing phases.
Bursitis
Inflammation of the bursa, a fluid-filled sac that reduces friction between bones,
tendons, and muscles. Subacromial bursitis is common in the shoulder, causing pain with
movement, especially overhead.
Dislocation/Subluxation
When the humerus completely comes out of the shoulder socket (dislocation) or partially
comes out (subluxation). This is often due to trauma and can damage surrounding
ligaments.
AC Joint Sprain/Separation
Injury to the acromioclavicular (AC) joint, where the collarbone (clavicle) meets the
shoulder blade (scapula), often caused by a direct fall onto the shoulder.
Osteoarthritis
Degenerative "wear and tear" of the shoulder joint cartilage, leading to pain,
stiffness, and reduced movement, more common in older adults.
2. Common Mechanism of Injury
Shoulder pain frequently results from
Overuse/Repetitive Strain
- Sports : Repetitive overhead activities in sports like swimming, tennis, baseball,
volleyball, or weightlifting.
- Occupational Activities : Jobs requiring frequent overhead work, heavy lifting, or
sustained arm positions (e.g., painters, carpenters, hairstylists).
Acute Trauma/Falls
- Falls onto an Outstretched Arm : A common cause of rotator cuff tears, dislocations,
or fractures.
- Direct Impact : A direct blow to the shoulder from a fall, collision, or contact
sport.
Poor Posture
Prolonged slouching or rounded shoulders can alter shoulder mechanics, leading to
impingement and rotator cuff strain over time.
Muscle Imbalance/Weakness
Imbalances between stronger chest muscles and weaker back/rotator cuff muscles can lead
to instability and injury.
Degeneration
Age-related wear and tear on tendons, cartilage, and joints.
3. Common Symptoms
Symptoms of shoulder pain vary widely depending on the
underlying cause.
They may include
Localised Pain
Aching, throbbing, or sharp pain in the shoulder joint, front, side, or sometimes
radiating down the arm.
Pain with Movement
Aggravated by specific arm movements, especially overhead lifting, reaching behind the
back, or rotating the arm.
Stiffness and Reduced Range of Motion
Difficulty lifting the arm, reaching, or performing daily tasks like dressing or hair
care.
Weakness
Difficulty lifting or rotating the arm, or feeling of "giving way."
Clicking, Popping, or Grinding Sounds
With shoulder movement, particularly with joint instability or degeneration.
Difficulty Sleeping
Pain aggravated by lying on the affected side.
Numbness or Tingling (less common for pure shoulder
issues)
May occur if nerve compression is present, possibly from the neck.
4. How Physiotherapy Can Help with Shoulder Pain
Physiotherapy is exceptionally effective in diagnosing, treating, and
preventing recurrence of shoulder pain, helping you regain strength, mobility, and function.
Our comprehensive approach focuses on identifying the specific cause of your pain and
empowering you with strategies for lasting recovery.
Here's how physiotherapy can help
Thorough Assessment
A detailed examination of your shoulder complex, neck, upper back, and posture to
pinpoint the source of your pain, assess muscle strength, joint mobility, movement
patterns, and identify contributing factors.
Pain Relief Strategies
- Manual Therapy : Hands-on techniques such as soft tissue massage, joint mobilisation
(including the shoulder, neck, and upper back), and stretches to reduce muscle spasm,
improve joint movement, and alleviate pain.
- Dry Needling/Acupuncture : Can be used to release trigger points in tight shoulder and
upper back muscles that contribute to pain and stiffness.
- Modalities : Application of heat, ice, or electrotherapy (like TENS) to help reduce
pain and inflammation during acute phases.
Restoring Movement & Strength
- Targeted Exercise Prescription : We design a personalised exercise program to
strengthen weak rotator cuff muscles, scapular stabilisers, and surrounding musculature,
while stretching tight structures to restore full range of motion.
- Graded Exposure & Progressive Loading : Guiding you through safe and progressive
exercises to improve tolerance to movement and gradually increase the load on your
shoulder.
- Movement Pattern Retraining : Correcting inefficient or painful movement patterns to
optimise shoulder mechanics during daily activities and sports.
Postural Correction & Ergonomic Advice
Guidance on maintaining optimal posture and assessing your workspace, sleeping habits,
and recreational activities to suggest modifications that support shoulder health and
prevent future injuries.
Education & Self-Management
Empowering you with a clear understanding of your condition, pain triggers, and
effective self-management techniques. This includes teaching you specific exercises,
stretches, and activity modification strategies you can use at home to maintain progress
and prevent re-injury.
Pre and Post-Surgical Rehabilitation
If surgery is required, we provide structured rehabilitation programs to optimise
recovery, restore function, and ensure a safe return to desired activities.
By addressing the underlying issues, improving mechanics, and providing you with the tools for self-care, physiotherapy aims to reduce your shoulder pain, restore full function, and help you return to your daily activities, work, and sports pain-free.

Elbow / forearm
1. What It Is & Common Types
The elbow is a complex hinge joint, allowing for bending and straightening
of the arm, while the forearm's two bones (radius and ulna) permit rotation of the hand.
This region is vital for gripping, lifting, carrying, and performing fine motor tasks. It's
stabilised by strong ligaments, and numerous muscles originating in the forearm cross the
elbow joint to control hand and wrist movements. Pain in the elbow or forearm often results
from overuse, repetitive strain, or direct trauma affecting these intricate structures.
Common types of elbow/forearm pain and related issues include
Lateral Epicondylitis (Tennis Elbow)
This is the most common condition, characterised by pain on the outer side of the elbow
where the forearm extensor muscles attach. It's caused by overuse and repetitive
gripping, wrist extension, or forearm rotation, leading to degeneration of the tendon.
Medial Epicondylitis (Golfer's Elbow)
Less common than tennis elbow, this involves pain on the inner side of the elbow where
the forearm flexor and pronator muscles attach. It's typically due to repetitive wrist
flexion, gripping, or forearm pronation.
Cubital Tunnel Syndrome
Occurs when the ulnar nerve, which passes through the cubital tunnel on the inner side
of the elbow, becomes compressed or irritated. This can cause numbness, tingling, or
weakness in the little finger and half of the ring finger, and sometimes pain in the
forearm.
Radial Tunnel Syndrome
Compression of the radial nerve in the forearm, often causing aching pain on the top or
outer side of the forearm, similar to tennis elbow but usually without local tenderness.
Olecranon Bursitis (Student's Elbow)
Inflammation of the bursa located over the bony tip of the elbow (olecranon). It often
presents as swelling, tenderness, and sometimes pain, usually caused by direct trauma or
prolonged leaning on the elbow.
Ligament Sprains
Injuries to the ligaments supporting the elbow joint, often from falls or overuse,
particularly in throwing athletes (e.g., UCL injury).
Osteoarthritis
Degenerative "wear and tear" of the elbow joint cartilage, less common than in other
major joints but can occur, especially in those with a history of trauma or heavy use.
2. Common Mechanism of Injury
Elbow and forearm pain frequently results from
Overuse & Repetitive Strain (Most Common)
- Sports : Repetitive gripping, throwing, swinging (tennis, golf, baseball, racket
sports), or weightlifting.
- Occupational Activities : Jobs requiring repetitive hand/wrist movements, gripping,
using tools (e.g., carpenters, plumbers, chefs, computer users, hairdressers).
Sudden Trauma/Impact
- Falls onto an Outstretched Arm : Can lead to fractures, dislocations, or ligament
sprains around the elbow.
- Direct Blow : An impact directly to the elbow or forearm.
Poor Ergonomics
Improper setup of workspaces, tools, or sports equipment leading to awkward postures or
excessive strain on the forearm muscles.
Muscle Imbalance/Weakness
Weakness in the muscles supporting the forearm and wrist can lead to overload of the
tendons around the elbow.
Nerve Compression
Sustained pressure or repeated stretching of nerves (e.g., ulnar nerve in the cubital
tunnel).
3. Common Symptoms
Symptoms of elbow and forearm pain can vary depending on
the underlying cause.
They may include
Localised Pain
Aching, sharp, or burning pain on the outer (tennis elbow) or inner (golfer's elbow)
side of the elbow. Pain can also be felt along the forearm.
Pain with Movement
Aggravated by gripping, lifting, carrying, twisting the forearm, or extending/flexing
the wrist.
Tenderness
Pain upon touching specific bony points around the elbow or along the forearm muscles.
Weakness
Difficulty gripping objects, turning doorknobs, or lifting.
Stiffness
Reduced range of motion in the elbow or wrist.
Numbness, Tingling, or Burning
If a nerve is compressed (e.g., Cubital Tunnel Syndrome), these sensations may radiate
into the hand (specifically the little and ring fingers for ulnar nerve).
Swelling
Especially with bursitis or acute trauma.
4. How Physiotherapy Can Help with Elbow & Forearm Pain
Physiotherapy is highly effective in diagnosing, treating, and
preventing recurrence of elbow and forearm pain, helping you regain strength, mobility, and
function. Our comprehensive approach focuses on identifying the specific cause of your pain,
addressing contributing factors, and empowering you with strategies for lasting recovery.
Here's how physiotherapy can help
Thorough Assessment
A detailed examination of your elbow, forearm, wrist, hand, shoulder, and neck to
pinpoint the source of your pain. We'll assess muscle strength, joint mobility, nerve
function, and identify aggravating activities and ergonomic factors.
Pain Relief Strategies
- Manual Therapy : Hands-on techniques such as soft tissue massage, trigger point
release, joint mobilisation of the elbow, wrist, and even the neck / upper back if
contributing.
- Dry Needling/Acupuncture : Can be used to release stubborn trigger points in tight
forearm muscles.
- Modalities : Application of heat, ice, electrotherapy (like TENS), or therapeutic
ultrasound to help reduce pain and inflammation during acute phases.
Restoring Movement & Strength
- Targeted Exercise Prescription : We design a personalised exercise program to
strengthen weak forearm, wrist, and grip muscles, while stretching tight structures to
improve flexibility and range of motion. This often includes eccentric exercises for
tendinopathies.
- Graded Exposure & Progressive Loading : Guiding you through safe and progressive
exercises and activities to improve tissue tolerance and gradually increase the load on
your elbow/forearm.
- Movement Pattern Retraining : Correcting inefficient or painful movement patterns
during daily activities, work, or sports.
Ergonomic & Activity Modification Advice
Guidance on optimising your workspace, tool use, sports technique, and daily habits to
reduce strain on your elbow and prevent future flare-ups. This includes advice on proper
grip, posture, and lifting techniques.
Education & Self-Management
Empowering you with a clear understanding of your condition, pain triggers, and
effective self-management techniques. This includes teaching you specific exercises,
stretches, and activity modification strategies you can use at home.
Bracing/Taping Advice
Recommendation and application of supportive bracing or taping if beneficial for pain
relief and support during recovery.
Nerve Gliding Exercises
Specific exercises to improve the mobility of compressed or irritated nerves.
By addressing the underlying issues, improving mechanics, and providing you with the tools for self-care, physiotherapy aims to reduce your elbow/forearm pain, restore full function, and help you return to your daily activities, work, and sports pain-free.

Wrist / hand
1. What It Is & Common Types
The Wrist and Hand complex consists of 27 small bones, numerous joints, ligaments, tendons,
and nerves, making it a masterpiece of fine motor control and dexterity. The wrist (carpus)
acts as a flexible bridge between the forearm and the hand, allowing for a wide range of
movements. The hand is essential for gripping, feeling, and performing countless daily
tasks. Pain arises when any of these structures are strained, inflamed, or compressed.
Common types of wrist and hand pain and related issues include
Carpal Tunnel Syndrome (CTS)
The most common nerve entrapment condition, where the median nerve is compressed as it
passes through the wrist tunnel. This causes pain, numbness, and tingling, typically in
the thumb, index, middle, and half of the ring finger.
De Quervain's Tenosynovitis
Inflammation of the tendons on the thumb side of the wrist, often caused by repetitive
gripping, lifting, or twisting motions. It causes pain and tenderness when moving the
thumb or wrist.
Tendonitis / Tenosynovitis
Inflammation or irritation of any of the many tendons that control finger and wrist
movement, often due to overuse.
Arthritis
- Osteoarthritis (OA) : "Wear and tear" typically affecting the base of the thumb (CMC
joint) or finger joints, causing pain, stiffness, and bony enlargement.
- Rheumatoid Arthritis (RA) : An autoimmune condition often affecting the small joints
of the hand and wrist symmetrically, causing pain, swelling, and potential joint
deformity.
Trigger Finger/Thumb (Stenosing Tenosynovitis)
A condition where a tendon sheath becomes inflamed, causing the finger or thumb to
catch, lock, or pop when attempting to straighten it.
Sprains and Fractures
Acute injuries, such as a Scaphoid fracture (a common wrist bone fracture often
resulting from a fall onto an outstretched hand) or ligament sprains.
2. Common Mechanism of Injury
Wrist and hand pain often results from
Repetitive Strain and Overuse
Activities involving prolonged or repeated gripping, typing, texting, assembly line
work, or use of hand tools. This is a primary cause of conditions like CTS and De
Quervain's.
Sudden Trauma / Falls
- Falling Onto an Outstretched Hand : A very common mechanism for spraining wrist
ligaments or fracturing bones (like the scaphoid or distal radius).
Awkward / Sustained Positions
Holding the wrist bent for long periods, such as when sleeping, working with
non-ergonomic tools, or poor keyboard/mouse setup.
Systemic Conditions
Underlying inflammatory conditions (like Rheumatoid Arthritis) or metabolic issues (like
Diabetes) can predispose individuals to nerve entrapment or tendon irritation.
Sports Injuries
Repetitive impact or rotational forces common in sports like golf, tennis, or contact
sports can lead to tendon and ligament damage.
3. Common Symptoms
Symptoms of wrist and hand pain can range from a dull ache to debilitating
sharp pain and functional loss.
They may include
Pain
Aching, burning, or sharp pain localised to the wrist, a specific finger, the thumb, or
radiating into the forearm.
Numbness and Tingling
Often following a specific nerve path (e.g., in the fingers and hand with Carpal Tunnel
Syndrome), often worse at night.
Weakness
Difficulty with grip strength, dropping objects, or struggling with fine motor tasks
(like buttoning a shirt or opening jars).
Stiffness and Reduced Mobility
Trouble making a full fist, limited ability to bend the wrist, or pain with specific
movements.
Swelling and Tenderness
Localised puffiness or extreme pain when pressing on a specific area (e.g., over an
inflamed tendon).
Clicking, Catching, or Locking
A sensation that a finger or the wrist joint is momentarily stuck, often associated with
Trigger Finger or underlying joint instability.
Visible Deformity or Bumps
May indicate a ganglion cyst, arthritis, or an old fracture site.
4. How Physiotherapy Can Help with Wrist & Hand Pain
Physiotherapy plays a crucial role in treating acute injuries and
chronic conditions of the wrist and hand, often providing an effective alternative to
injections or surgery. Our goal is to relieve pain, restore full function and dexterity, and
enable you to confidently resume all your daily and work activities.
Here's how physiotherapy can help
Thorough Assessment and Diagnosis
We conduct a detailed examination, including specialised orthopaedic tests, nerve
tension checks, grip strength assessment, and evaluation of your daily postures and work
habits, to pinpoint the exact structure causing the pain.
Pain and Swelling Reduction
- Manual Therapy : Gentle joint mobilisation and soft tissue techniques to reduce
swelling, improve joint movement, and alleviate muscle tension in the forearm.
- Activity Modification : Identifying and adjusting painful activities or movements to
allow irritated structures to heal.
- Taping / Bracing / Splinting : Applying temporary support or providing custom
recommendations for braces/splints to offload aggravated nerves or tendons (e.g., for
CTS or De Quervain's).
Restoring Strength, Movement, and Dexterity
- Targeted Exercise Prescription : Custom exercises to restore range of motion, improve
grip and pinch strength, and enhance the fine motor control needed for delicate tasks.
- Tendon and Nerve Gliding Exercises : Specific movements to help irritable tendons and
nerves slide smoothly within their tunnels, reducing friction and compression (highly
effective for CTS and tendonitis).
Ergonomic and Posture Advice
Evaluating your work desk setup, tools, or hobbies (e.g., keyboard, mouse, or phone use)
to suggest modifications that ensure a neutral and strain-free wrist posture.
Rehabilitation Post-Fracture or Surgery
Providing structured, progressive rehabilitation programs following a fracture or
procedure, ensuring the safe return of strength, movement, and functional independence.
By combining pain-relieving strategies with empowering strengthening exercises and ergonomic education, physiotherapy aims to resolve your symptoms, restore the full functionality of your hand and wrist, and prevent future recurrence.

Spinal Pain (Upper, Mid, and Lower Back)
1. What It Is & Common Types
The Spine is the central pillar of the body, encompassing the neck
(Cervical), mid-back (Thoracic), and lower back (Lumbar) regions. It provides structure,
allows for mobility, and protects the spinal cord. Pain arises when any of its complex
components—vertebrae, discs, joints, muscles, or nerves—become irritated or damaged.
Common conditions we treat across the spine include
Lower Back (Lumbar)
Sciatica / Radiculopathy (Pinched Nerve), Herniated Disc, Mechanical Low Back Pain,
Spinal Stenosis, Spondylolisthesis.
Mid Back (Thoracic)
Postural Pain, Scheuermann’s Disease, Rib Pain/Joint Dysfunction, Stiffness
(Hypomobility), referred pain from the neck.
Upper Back / Shoulders
Muscle Strain (e.g., Rhomboids/Trapezius), Shoulder Blade Pain, Tension Headaches
(originating from the neck/upper back), Thoracic Outlet Syndrome.
2. Common Mechanism of Injury
Spinal pain often results from a combination of forces and habits
Poor Posture and Prolonged Positions
Slouching while sitting, working at a desk with an incorrect setup, or "text neck" puts
chronic, uneven strain on all spinal segments, especially the Mid and Upper Back.
Improper Lifting / Twisting
Sudden, forceful, or repetitive movements, particularly when lifting with a rounded
spine, commonly injure the muscles, discs, and joints of the Lower Back.
Repetitive Strain and Overuse
Activities that involve repeated bending, reaching, or rotating (common in manual labour
or sports) can strain the surrounding muscles and ligaments in any spinal region.
Weak Core and Stabilising Muscles
Insufficient strength in the deep core, hip, and shoulder blade muscles means the spine
lacks stable support, leading to overuse of other structures.
Trauma
Falls, accidents, or sudden impacts can cause acute sprains, whiplash (affecting the
upper back/neck), or fractures.
Stress
High stress levels frequently lead to chronic tension and muscle guarding in the Upper
Back and shoulders, triggering pain and headaches.
3. Common Symptoms
Symptoms of back pain are highly varied based on the location
Localised Pain
A dull ache, sharp stiffness, or burning sensation felt specifically at the site of the
pain (e.g., right between the shoulder blades, or deep in the lumbar area).
Radiating Pain
Pain, numbness, or tingling that travels down the leg (Sciatica - from the lower back)
or down the arm (from the upper back / neck junction).
Stiffness and Reduced Motion
Difficulty bending, standing up straight, looking over the shoulder, or sitting
comfortably for long periods (common across all regions).
Rib or Chest Pain
Sharp, localised pain when taking a deep breath, coughing, or twisting, often indicating
Mid Back (thoracic) joint or rib irritation.
Headaches
Tension or cervicogenic headaches that start at the base of the skull and refer over the
head, stemming from Upper Back / Neck tightness.
Muscle Spasm
Involuntary, painful tightening and knotting of the large spinal muscles, often severely
limiting movement.
4. How Physiotherapy Can Help with Spinal Pain
Physiotherapy is the most effective and recommended non-surgical
treatment for the vast majority of spinal issues. Our goal is to relieve your immediate
pain, restore healthy movement patterns, and give you the strength and knowledge to prevent
recurrence.
Here's how physiotherapy can help across the entire back
Thorough Assessment
We conduct a detailed examination of your posture, movement mechanics, core stability,
and nerve function to pinpoint the root cause of your pain, not just the symptoms.
Pain Relief Strategies
- Manual Therapy : Hands-on techniques, including massage, joint mobilisations, and
specific spinal manipulation, to release muscle tension, restore mobility to stiff
segments (especially the Mid Back), and reduce nerve irritation.
- Dry Needling / Acupuncture : Used to release painful trigger points and muscle knots
in the tight muscles of the Upper and Lower Back.
Restoring Stability and Movement
- Targeted Exercise Prescription : A personalised program focusing on strengthening the
deep core stabilisers (for the lower spine) and the scapular stabilisers (for the upper
spine). This provides a resilient foundation for the entire back.
- Mobility Exercises : Specific movements and stretches to improve the flexibility of
the thoracic spine and hips, which often compensate for poor posture.
Ergonomic and Postural Correction
Guidance on achieving optimal posture while sitting, standing, and lifting. This
includes evaluating your office or work setup to eliminate chronic strain triggers in
the neck and mid-back.
Nerve Pain Management
Specific positions, stretches, and nerve gliding techniques designed to gently de-stress
and manage the symptoms of Sciatica or arm pain originating from the spine.
Education and Self-Management
Empowering you with a clear understanding of your body, proper body mechanics for daily
tasks (e.g., safe lifting), and a comprehensive home exercise program to maintain your
progress and confidently manage your back health long-term.
By integrating targeted pain relief strategies (including manual therapy) with restorative exercise prescription and ergonomic education, physiotherapy aims to resolve spinal symptoms, restore optimal function across the entire back, and empower you with the self-management tools necessary for long-term prevention of recurrence.

Hip / groin
1. What It Is & Common Types
The Hip Joint is one of the body's largest weight-bearing joints—a
stable ball-and-socket structure connecting the pelvis and the thigh bone (femur). It's
designed for powerful movement and stability during standing, walking, and running. The
Groin refers to the area where the abdomen meets the thigh, housing major muscles, tendons,
and ligaments that support the hip and leg. Pain here is complex, often arising from the
joint itself or surrounding soft tissues.
Common types of hip and groin pain and related
issues include
Osteoarthritis (OA)
The progressive "wear and tear" of the cartilage lining the hip socket, leading to deep,
aching pain, stiffness, and reduced rotation, often felt in the groin area.
Gluteal Tendinopathy / Bursitis (Greater Trochanteric Pain
Syndrome)
Pain and tenderness on the outer side of the hip/thigh, often caused by compression and
overuse of the gluteal tendons (especially the Gluteus Medius). Bursitis often occurs
alongside it.
Hip Flexor Strain
A tear or overstretching of the muscles at the front of the hip (like the Iliopsoas),
common in athletes requiring explosive leg movements (e.g., kicking, sprinting).
Hip Labral Tear
An injury to the ring of cartilage (labrum) surrounding the hip socket. This can cause
sharp, catching, or clicking pain deep in the groin, often aggravated by deep bending or
twisting.
Adductor (Groin) Strain
Injury to the inner thigh muscles, resulting in pain in the inner groin, typically
sustained during sudden sideways movements or lunging.
Femoroacetabular Impingement (FAI)
A condition where extra bone growth on the hip socket or femoral head causes abnormal
contact, leading to joint damage and pain with hip flexion.
2. Common Mechanism of Injury
Hip and groin pain often results from
Overuse and Repetitive Load
Running, cycling, or climbing stairs can cause cumulative stress, leading to conditions
like tendinopathy (glutes, hip flexors) or OA over time.
Sudden, Explosive Movements
Sprinting, kicking, or rapid changes of direction place immense strain on the groin and
hip flexor muscles, often resulting in acute muscle strains / tears.
Trauma / Falls
Direct falls onto the side of the hip (causing bursitis or fractures) or impacts that
force the hip into an awkward position.
Biomechanical Imbalances
Weakness in key stabilising muscles, particularly the Gluteal muscles, which causes the
hip joint to move incorrectly, leading to strain on the joint and surrounding tendons.
Prolonged Sitting
Spending long periods in a seated position can shorten the hip flexor muscles, altering
pelvic posture and increasing the risk of strain when standing or exercising.
Age-Related Degeneration
The natural process of wear and tear that is the primary contributor to Osteoarthritis.
3. Common Symptoms
Symptoms of hip and groin pain can be confusing, as pain from the hip
joint often refers to the groin.
They may include
Localised Deep Pain
A deep ache felt inside the groin or buttock, often a sign that the pain is coming from
the hip joint itself (e.g., OA or FAI).
Pain on the Side of the Hip
Tenderness and pain felt directly on the bony prominence on the side of the hip (the
greater trochanter), often worse when lying on that side or walking (Gluteal
Tendinopathy / Bursitis).
Inner Thigh Pain
Pain along the inside of the leg, especially when bringing the legs together or
stretching them apart (Adductor / Groin Strain).
Stiffness and Restricted Motion
Difficulty tying shoelaces, putting on socks, or crossing the legs due to limited hip
rotation or bending.
Clicking, Catching, or Locking
Sensations felt deep in the hip joint, often associated with a Labral Tear or FAI.
Pain with Weight-Bearing
Increased pain when walking, standing, or shifting weight onto the affected leg.
Referred Pain
Pain that travels down the front of the thigh to the knee, often mistaken for a primary
knee problem.
4. How Physiotherapy Can Help with Hip & Groin Pain
Physiotherapy is essential for accurate diagnosis and effective
rehabilitation of hip and groin conditions, focusing on pain relief, restoring range of
motion, and building powerful stability from the core down to the knee.
Here's how
physiotherapy can help
Thorough Assessment and Diagnosis
We conduct a detailed examination, including specialised movement tests, analysis of
your walking/running pattern (gait analysis), and assessment of hip and core strength to
accurately distinguish between joint, tendon, and muscular sources of pain.
Pain Relief and Inflammation Management
- Manual Therapy : Hands-on techniques, including deep tissue release to tight muscles
(e.g., hip flexors, deep rotators) and gentle joint mobilisations to improve hip joint
health and reduce stiffness.
- Activity Modification : Identifying and adjusting activities (e.g., running technique,
sitting positions) that aggravate the hip or groin to allow irritated structures to
heal.
- Modalities : Using ice or heat to manage acute pain and tendon inflammation.
Restoring Stability and Strength
- Targeted Exercise Prescription : The core of recovery, focusing intensely on
strengthening the crucial Gluteal muscles (Medius and Maximus), which are vital for
controlling hip and pelvic stability during movement.
- Core and Pelvic Stability Training : Exercises to integrate the core and hip muscles,
ensuring the pelvis remains stable during high-load activities.
Improving Flexibility and Biomechanics
Specific stretching exercises to address common tightness in the hip flexors and
adductors, along with guidance on improving squatting and lifting mechanics to reduce
stress on the joint.
Osteoarthritis and FAI Management
Providing education and a carefully graded exercise program proven to reduce pain and
delay the progression of joint issues by maintaining strength and mobility.
Return to Sport Rehabilitation
Developing a structured, progressive program with advanced agility and power drills to
safely restore function after strains or tears, minimising the risk of recurrence.
By addressing biomechanical faults and building robust strength around this powerful joint, physiotherapy aims to resolve your pain, restore your full range of movement, and help you return to your fitness goals and daily life without limitation.

Thigh
1. What It Is & Common Types
The Thigh is the largest and strongest segment of the lower limb,
centred around the femur (thigh bone). It is home to the body's largest muscle groups: the
Quadriceps (front), the Hamstrings (back), and the Adductors (inner thigh/groin). These
powerful muscles are vital for walking, running, jumping, and stability. Thigh pain
typically stems from muscle, tendon, or bone injury, or is often referred from the hip or
lower back.
Common types of thigh pain and related issues include
Muscle Strains
Tears in the muscle fibres, categorised by location and severity.
- Hamstring Strain : The most common athletic thigh injury, causing sharp pain and
tenderness at the back of the thigh, often occurring during sprinting or explosive
movements.
- Quadriceps Strain : Affecting the front of the thigh, often the Rectus Femoris muscle,
common in kicking sports or sudden acceleration.
- Adductor (Groin) Strain : Affecting the inner thigh muscles, causing pain during
side-to-side movements or when bringing the legs together.
Contusion (Corked Thigh / Dead Leg)
A severe bruise resulting from a direct, blunt impact to the muscle, causing bleeding,
deep pain, and swelling (haematoma) in the muscle belly, most common in the Quadriceps.
Iliotibial Band (ITB) Syndrome
Although primarily causing outer knee pain, the ITB itself is a thick fibrous band
running along the outer thigh. Irritation can cause pain and snapping sensation along
the side of the thigh and hip.
Referred Pain
Pain felt in the thigh, but originating from the lower back (e.g., Sciatica or Femoral
Nerve irritation) or the hip joint (e.g., Osteoarthritis).
2. Common Mechanism of Injury
Thigh pain often results from
Sudden, High-Speed Contraction
- Sprinting : Accelerating or reaching maximum speed is a classic mechanism for
Hamstring Strains.
- Kicking / Jumping : Explosive hip flexion and knee extension can cause Quadriceps
Strains.
Direct Trauma
A forceful collision or blow (e.g., knee-to-thigh impact in contact sports) leads to a
Contusion (Corked Thigh).
Overstretching / Sudden Change of Directio
Lunging, slipping, or rapid directional changes place extreme tension on the Hamstrings
and Adductors.
Overuse and Biomechanics
Repetitive use without adequate rest, or underlying issues like muscle imbalance (e.g.,
Hamstrings weaker than Quads), poor running technique, or weak gluteal muscles, can
contribute to strains and ITB issues.
Inadequate Warm-up or Fatigue
Muscles that are cold or fatigued are less able to absorb load, making them
significantly more vulnerable to strain and tearing.
3. Common Symptoms
Symptoms of thigh pain can vary greatly, from a deep bruise to a debilitating sharp tear
Sharp, Sudden Pain
An immediate, severe sensation often described as a "pop" or "snap" during a dynamic
activity, which is a key sign of a muscle tear (strain).
Pain with Muscle Contraction
Pain when trying to flex the knee (Hamstrings) or extend the knee (Quadriceps), or when
trying to squeeze the legs together (Adductors).
Bruising and Swelling
Visible discolouration (bruising) and palpable lump or swelling at the site of injury,
especially with severe strains or contusions.
Difficulty Weight-Bearing
Inability or severe pain when walking, running, or standing on the affected leg.
Stiffness and Tightness
A feeling of tightness or restricted movement, particularly when trying to stretch the
injured muscle.
Numbness, Tingling, or Burning
Sensations that can indicate nerve irritation, often signifying that the pain is
referred from the lower back (Sciatica or Femoral Nerve involvement).
Pain with Sitting
Discomfort or pain in the back of the thigh / buttock, which can sometimes indicate a
high (proximal) Hamstring Tendinopathy.
4. How Physiotherapy Can Help with Thigh Pain
Physiotherapy is critical for the accurate diagnosis, optimal healing,
and functional rehabilitation of thigh injuries, helping to minimise the risk of re-injury.
Our phased approach respects the tissue healing time while ensuring the muscle regains full
strength and power.
Here's how physiotherapy can help
Accurate Diagnosis and Early Management (R.I.C.E.)
We precisely assess the location and severity (Grade 1, 2, or 3) of the muscle strain or
contusion. Initial treatment focuses on rest, controlled ice, compression, and elevation
to manage swelling and restrict bleeding, which is vital for a good outcome.
Pain Relief and Tissue Healing
- Soft Tissue Release : Gentle manual therapy to reduce muscle guarding and tension in
adjacent areas.
- Modalities : Use of therapeutic ultrasound or electrotherapy (if appropriate) to
promote muscle tissue repair.
- Activity Guidance : Clear advice on when and how to start moving the injured leg
without compromising the healing tissue.
Phased Strength and Flexibility Restoration
- Restoring Range of Motion (Phase 1) : Gentle, pain-free mobility exercises to prevent
excessive scar tissue formation and stiffness.
- Progressive Strengthening (Phase 2 & 3) : A carefully graded exercise program,
starting with light isometric (static) exercises and progressing to powerful, eccentric
(lengthening) loading and high-speed functional movements, which is essential to
bulletproof the muscle against future strains.
Biomechanical and Running Analysis
We evaluate your walking, running, or sport-specific technique to identify predisposing
factors like pelvic instability, poor foot mechanics, or muscle imbalances between the
quadriceps and hamstrings.
Prevention and Return to Sport
Developing a customised maintenance program that includes specific strength and
flexibility exercises (like the Nordic Hamstring Curl) to minimise recurrence. We guide
you through a structured, safe return-to-sport progression, ensuring your thigh has the
power and endurance needed for your specific activity.
By employing specific strengthening and loading protocols, physiotherapy aims to ensure the injured thigh muscle heals strong, flexible, and fully capable of handling the demands of daily life and sport.

Knee
1. What It Is & Common Types
The Knee is the largest and one of the most complex joints in the
body, connecting the thigh bone (femur) to the shin bone (tibia). It also includes the
kneecap (patella), which sits in front. The knee is stabilised by four main ligaments
(cruciates and collaterals) and cushioned by two pieces of cartilage (menisci). It's
designed to bear weight and allow for smooth movement during walking, running, jumping, and
squatting. Knee pain arises when any of these structures are irritated, inflamed, or
damaged.
Common types of knee pain and related issues include
Osteoarthritis (OA)
A "wear and tear" condition where the cartilage cushioning the joint gradually breaks
down, leading to pain, stiffness, and swelling. It is the most common form of knee
arthritis.
Patellofemoral Pain Syndrome (PFPS)
Often called "runner's knee," this is pain around or under the kneecap. It's usually
caused by repetitive stress or incorrect tracking of the kneecap, often due to muscle
imbalances in the hip or thigh.
Meniscal Tears
Injury to the C-shaped cartilage in the knee, often caused by a sudden twisting motion
while the foot is planted. Symptoms include sharp pain, swelling, and sometimes a
locking or catching sensation.
Ligament Sprains / Tears
Injuries to the crucial stabilising ligaments, such as the ACL (Anterior Cruciate
Ligament) or MCL (Medial Collateral Ligament), typically resulting from direct impact or
sudden changes in direction during sport.
Tendonitis / Tendinopathy
Inflammation or irritation of the tendons around the knee, such as the Patellar Tendon
(Jumper's Knee) or Quadriceps Tendon, usually due to overuse or a sudden increase in
activity.
2. Common Mechanism of Injury
Knee pain and injury often result from
Overuse and Repetitive Stress
Activities involving repeated bending or loading of the knee, such as running, cycling,
or stair climbing, which can lead to tendonitis or PFPS.
Sudden Trauma / Twisting
- Sports Injuries : Direct blows to the knee, landing awkwardly from a jump, or sudden
stopping and pivoting movements (common in soccer, basketball, skiing) are frequent
causes of ligament and meniscal tears.
- Falls : Landing directly on the knee or twisting the leg during a fall.
Biomechanical Issues
Problems with alignment or movement patterns that put excessive or abnormal strain on
the knee joint. This often relates to weak hip or core muscles, or flat feet.
Age-Related Degeneration
The natural wear and tear process that contributes to conditions like Osteoarthritis.
Sustained Positions
Prolonged kneeling or squatting, which can put excessive pressure on the joint
structures.
3. Common Symptoms
Symptoms of knee pain can vary widely depending on the underlying
structure involved.
They may include
Localised Pain
A dull ache, sharp stabbing pain, or burning sensation in, around, or behind the
kneecap.
Swelling and Inflammation
Fluid build-up around the joint, making it appear puffy or warm to the touch
Stiffness
Difficulty fully bending or straightening the knee, often worse after periods of rest or
in the morning (common with OA).
Instability ("Giving Way")
A feeling that the knee is unreliable or might buckle, often associated with ligament
injuries.
Clicking, Popping, or Grinding
Sounds or sensations during movement (crepitus), particularly if cartilage or the
meniscus is involved.
Locking or Catching
A feeling that the knee is momentarily stuck, which can be a sign of a meniscal tear.
Difficulty with Activities
Pain or inability to climb stairs, squat, run, or tolerate standing for long periods.
4. How Physiotherapy Can Help with Knee Pain
Physiotherapy is the primary treatment for most knee conditions and is
highly effective in reducing pain, restoring mobility, and helping you avoid surgery (where
possible). Our approach focuses on not just treating the knee but also addressing underlying
issues in the hip and foot that contribute to the problem.
Here's how physiotherapy can
help
Thorough Assessment
We will conduct a detailed examination of your knee, hip, ankle, and walking/running
mechanics to accurately diagnose the injury and identify biomechanical factors
contributing to your pain (e.g., poor muscle activation or alignment).
Pain and Swelling Management
- Manual Therapy : Gentle joint mobilisations to improve movement and reduce stiffness,
and soft tissue release to relieve muscle tension around the thigh and calf.
- Modalities : Use of ice, heat, or TENS to manage acute pain and swelling.
Restoring Strength and Stability
- Targeted Exercise Prescription : We design a personalised program to strengthen
crucial muscles like the quadriceps, hamstrings, and, most importantly, the hip
stabilisers (glutes). Stronger hip muscles help control the knee's movement and
alignment.
- Balance and Proprioception Training : Specific exercises to improve your joint
awareness and reaction time, which is vital for preventing re-injury, especially after
ligament sprains.
Movement Correction and Biomechanics
- Gait Analysis : Assessing your walking or running style to identify and correct faulty
movement patterns that place stress on the knee.
- Foot / Ankle Management : Advice on footwear or referrals for custom orthotics if foot
mechanics are a contributing factor.
Activity Modification and Return to Sport
Guidance on how to safely modify your daily activities or training load as your knee
heals. We provide structured rehabilitation programs to ensure a safe and full return to
your job or sport, minimising the risk of future problems.
By treating the source of your pain and giving you the tools to manage your knee health, physiotherapy aims to reduce your pain, improve your mobility, and restore your confidence in moving well.

Shin / calf
1. What It Is & Common Types
The Shin and Calf make up the lower leg, connecting the knee to the
ankle and foot. The Shin (or tibia) is the large bone at the front, surrounded by muscle
groups responsible for lifting the foot (ankle dorsiflexion). The Calf is at the back,
dominated by the powerful Gastrocnemius and Soleus muscles, which are crucial for pushing
off the ground (plantarflexion) during walking and running. Pain here often involves bone
irritation (stress), muscle tears, or overuse of tendons.
Common types of shin and calf
pain and related issues include
Medial Tibial Stress Syndrome (MTSS)
Commonly known as Shin Splints. This is a painful, generalised condition involving
overuse and irritation of the tissues and bone surface along the inner edge of the shin
bone (tibia). It's very common in runners and those new to exercise.
Calf Muscle Strain / Tear
A rupture of the muscle fibres in the calf, often the Gastrocnemius, resulting in a
sudden, sharp pain usually felt during explosive movements like sprinting or jumping.
Often referred to as a "tennis leg."
Achilles Tendinopathy
An overuse injury causing pain, stiffness, and thickening of the large Achilles tendon
that connects the calf muscles to the heel bone.
Stress Fractures
A small crack in the bone (most commonly the tibia) caused by repetitive, excessive
force. Pain is highly localised and often worsens during activity and may be present at
rest.
Compartment Syndrome
A less common, but serious, condition where swelling or bleeding within the tight,
muscular compartments of the lower leg causes a dangerous build-up of pressure,
typically resulting in severe pain, tightness, and sometimes numbness.
2. Common Mechanism of Injury
Shin and calf pain often result from
Sudden Increase in Load / Intensity
A rapid jump in running mileage, pace, or frequency of exercise is the primary cause of
Shin Splints and Achilles Tendinopathy, as the tissues don't have time to adapt.
Change in Training Surface or Footwear
Running on hard surfaces (like concrete) or using worn-out or inappropriate running
shoes increases impact forces, stressing the shin bone and tendons.
Biomechanical Issues
Excessive foot pronation (flat feet) or weak hip/gluteal muscles alter the mechanics of
the lower leg, increasing rotation and strain on the shin and calf.
Explosive Movements
Sudden acceleration, lunging, or jumping can overload the calf muscles, leading to acute
tears (strains).
Inadequate Recovery
Not allowing sufficient rest between intense training sessions means muscles and bone
tissues cannot repair and strengthen, leading to cumulative overuse injuries.
3. Common Symptoms
Symptoms in the shin and calf can vary significantly depending on whether the injury is muscular, tendinous, or bony
Diffuse Pain
Generalised aching or burning along the inner border of the shin (MTSS/Shin Splints),
typically worse at the beginning of exercise and potentially subsiding, but returning
later.
Sharp, Localised Pain
Intense pain that begins abruptly during exercise, often accompanied by a "pop" or
"snap" sensation (Calf Strain/Tear).
Pinpoint Tenderness
Extreme sensitivity to touch over a small, specific area on the shin bone, which is a
key indicator of a Stress Fracture.
Stiffness and Tightness
A feeling of tension in the calf muscles, especially in the morning or after prolonged
rest, common with Achilles Tendinopathy.
Pain with Push-Off
Discomfort when pushing your toes off the ground or climbing stairs, due to pain in the
calf or Achilles tendon.
Swelling and Bruising
Visible swelling or bruising in the calf with a severe muscle tear.
Cramping/Numbness During Exercise
Tightness and cramping that builds rapidly during activity, forcing you to stop, which
may indicate Compartment Syndrome.
4. How Physiotherapy Can Help with Shin & Calf Pain
Physiotherapy is crucial for accurately identifying the cause of lower leg
pain (is it a muscle strain, shin splints, or a stress fracture) and implementing a safe,
phased return to activity. Our treatment focuses on healing, correcting underlying faults,
and preventing recurrence.
Here's how physiotherapy can help
Accurate Diagnosis and Load Management
We perform specific tests to differentiate between muscle tears, shin splints, and
potential stress fractures. We provide immediate guidance on modifying your training
load to allow the injured tissue to start healing effectively.
Pain and Inflammation Reduction
- Manual Therapy : Deep soft tissue massage, trigger point therapy, and gentle joint
mobilisations to relieve tension in the calf and surrounding muscles and reduce stress
on the shin bone.
- Taping : Application of supportive or muscle-facilitation taping to reduce strain on
the shin, calf, or Achilles tendon during the early phase of rehabilitation.
Biomechanical Correction and Strengthening
- Targeted Exercise Prescription : We design a personalised program to strengthen the
deep calf muscles, the shin muscles (to help lift the foot), and, crucially, the hip and
gluteal muscles to improve pelvic and knee control.
- Foot and Ankle Assessment : Evaluation of your foot posture (pronation/supination) and
providing advice on appropriate footwear or, if necessary, referring for orthotics to
correct faulty mechanics that contribute to shin pain.
Graded Exposure and Return to Activity
This is essential for all overuse injuries. We create a structured, progressive plan to
safely reintroduce running or exercise, monitoring symptoms closely to ensure tissues
adapt without becoming re-injured. This involves specific exercises to build tissue
tolerance.
Education and Prevention
Empowering you with knowledge about optimal running form, proper warm-up/cool-down
routines, and self-management strategies to maintain strong, injury-resistant lower legs
for the long term.
By addressing the specific cause of your pain and correcting the biomechanical factors that overload the lower leg, physiotherapy helps you recover fully and return to your activities safely and permanently.

Ankle and foot
1. What It Is & Common Types
The Ankle and Foot together contain 26 bones, 33 joints, and over 100
muscles, tendons, and ligaments, designed to absorb shock, adapt to uneven terrain, and act
as a rigid lever for pushing off. The Ankle Joint primarily allows for up-and-down movement
(plantar and dorsiflexion), while the numerous small joints in the foot allow for complex
arch adjustments and stability. Pain arises when these delicate structures are overstressed
or traumatised.
Common types of ankle and foot pain and related issues include
Ankle Sprains
The most common injury, occurring when the ankle is twisted or rolled, typically
damaging the ligaments on the outside of the ankle. Sprains are graded by severity.
Plantar Fasciitis
Inflammation and degeneration of the thick band of tissue (plantar fascia) that runs
across the bottom of the foot, connecting the heel bone to the toes. This causes sharp,
stabbing pain, often worst with the first steps in the morning.
Achilles Tendinopathy
Pain and stiffness in the Achilles tendon (connecting the calf to the heel), usually an
overuse injury common in runners, walkers, or those with tight calves.
Tendonitis (e.g., Peroneal or Tibialis Posterior)
Inflammation of the tendons that help control the arch and stabilise the ankle, usually
due to overuse or abnormal foot mechanics.
Bunion / Hallux Valgus
A bony bump that forms on the joint at the base of the big toe, causing pain, especially
with footwear.
Stress Fractures
Small cracks in the bones of the foot or ankle, often in the metatarsals, caused by
repetitive loading without adequate rest.
Morton's Neuroma
Thickening of the tissue around a nerve, usually between the third and fourth toes,
causing sharp, burning pain, numbness, or tingling in the toes, often aggravated by
tight shoes.
Foot Arch Pain / Collapse
Pain or discomfort due to issues with the foot's arches (e.g., flat feet, high arches),
which can affect shock absorption and weight distribution.
Referred Pain
Pain felt in the ankle or foot that originates from another area, most commonly the
lower back (e.g., sciatica radiating down the leg).
2. Common Mechanism of Injury
Ankle and foot pain often results from
Twisting / Rolling Accidents
Landing awkwardly from a jump, stepping into a hole, or slipping, which forces the ankle
into an unnatural position, leading to acute Ankle Sprains.
Overuse and Repetitive Impact
High-impact activities like running, marching, or prolonged standing, especially on hard
surfaces, are the primary drivers for Plantar Fasciitis, Achilles Tendinopathy, and
Stress Fractures.
Inappropriate Footwear
Wearing shoes that lack arch support, have poor cushioning, or high heels can
dramatically alter foot mechanics and increase stress on the tendons and fascia.
Biomechanical Faults
Underlying issues such as excessively flat feet (over-pronation) or high arches alter
the way forces are distributed during walking, contributing to overuse injuries.
Muscle Imbalance
Weakness in the stabilising muscles of the lower leg (like the Peroneals) makes the
ankle joint inherently unstable and prone to recurrent sprains.
3. Common Symptoms
Symptoms in the ankle and foot can vary greatly depending on the structure involved
Sharp, Immediate Pain & Swelling
A sudden onset of pain accompanied by rapid swelling and bruising, typically following a
twisting event (Ankle Sprain).
Morning Pain
Severe, sharp, stabbing pain on the bottom of the heel or foot with the first steps out
of bed or after sitting for a period (Plantar Fasciitis).
Pain with Push-Off
A dull ache or stiffness in the back of the heel and lower calf, especially when walking
up hills or stairs (Achilles Tendinopathy).
Instability
A feeling that the ankle is weak, "wobbly," or prone to giving way, especially when
walking on uneven ground (post-sprain instability).
Localised Tenderness
Extreme sensitivity and pain when pressing on a specific small area on a foot bone,
often worsening during activity (Stress Fracture).
Altered Walking Pattern
Limping or changing the way you walk to avoid putting pressure on a painful area.
4. How Physiotherapy Can Help with Ankle & Foot Pain
Physiotherapy is essential for effective treatment of both acute ankle
injuries and chronic foot overuse syndromes. Our approach focuses on restoring stability,
optimising foot mechanics, and building strong, resilient tissues to prevent future
problems.
Here's how physiotherapy can help
Thorough Assessment and Diagnosis
We conduct a detailed examination, including specific orthopaedic tests, gait analysis,
and assessment of your foot posture and footwear to accurately diagnose the injury and
identify underlying mechanical contributors.
Pain and Inflammation Reduction
- Manual Therapy : Gentle joint mobilisation to restore movement in the stiff ankle and
foot joints, and soft tissue release to tight calf muscles and restricted tendons.
- Taping & Bracing : Applying supportive taping techniques or providing recommendations
for walking boots/braces to protect healing ligaments and unload inflamed fascia or
tendons.
- Modalities : Use of ice, dry needling, or other modalities to manage acute pain and
swelling.
Restoring Stability and Strength
- Targeted Exercise Prescription : A carefully graded program focused intensely on
proprioception (balance) training to restore the body's awareness of the ankle's
position, which is crucial after a sprain.
- Strengthening : Exercises to strengthen the lower leg muscles (especially the peroneal
and calf muscles) to provide dynamic stability and support the arch.
Biomechanical Correction and Overuse Management
- Footwear and Orthotic Advice : Clear guidance on choosing appropriate shoes for
activity, and determining if temporary or custom orthotics are needed to support the
arch and correct faulty foot mechanics.
- Tissue Loading Program : For chronic conditions like Plantar Fasciitis and Achilles
Tendinopathy, we implement specific, evidence-based strengthening exercises designed to
gradually increase the tissue's tolerance to load.
Education & Self-Management
Empowering you with a clear understanding of your condition, common triggers, and
effective self-management strategies. Learning how to tape an ankle, perform exercises
correctly, and manage daily loads is key to long-term foot and ankle health.
Return to Sport Rehabilitation
Developing a structured program with agility and plyometric drills to ensure the ankle
can withstand high impact and changes in direction before a full return to sport.
By stabilising the joint, correcting biomechanical stressors, and strengthening the entire lower kinetic chain (foot, ankle, and hip), physiotherapy aims to resolve your pain, restore confidence in your balance, and ensure your feet and ankles can handle the demands of your active life.
- Podiatry
& Conditions Treated
- Nail Surgery
- Custom Foot Orthotics
- Dry Needling
- Footwear Assessment and Prescription
- Diabetes Foot Risk Assessment
- Paediatric Podiatry
- Corns, Callus & Wart Treatment
- Pressure Plate Analysis

Podiatry
Podiatry is a specialised discipline within allied health that focuses on the evaluation,
diagnosis, treatment, and prevention of disorders affecting the foot, ankle, and lower leg.
Podiatrists are highly skilled healthcare professionals who deliver comprehensive management
for individuals experiencing lower limb conditions.
With extensive training across areas such as anatomy, biomechanics, pharmacology, and
surgical principles, podiatrists are equipped to identify and treat a wide range of foot and
ankle issues. They utilise various diagnostic tools and methods, including gait analysis and
referrals for imaging such as X-rays and ultrasounds, to assess lower limb health and
function accurately.
Beyond addressing acute issues, podiatrists also support patients with chronic systemic
conditions such as diabetes, arthritis, and peripheral arterial disease, which can
significantly impact foot health. They provide guidance on preventive strategies, including
appropriate footwear choices, targeted exercises, and lifestyle modifications to minimise
future complications.
Ultimately, podiatry plays a vital role in preserving mobility, enhancing independence, and
improving overall quality of life. Through personalised care plans tailored to individual
needs, podiatrists contribute to maintaining optimal foot and ankle function across all age
groups.

Nail Surgery
(Partial or Total Nail Avulsion)
A minor surgical procedure to treat recurring or infected ingrown toenails. The affected portion (or whole nail) is removed under local anaesthetic, with the option for permanent removal using phenolisation.
Common Conditions Treated
Ingrown Toenail
Nail Infections

Custom Foot Orthotics
Individually prescribed insoles designed to correct biomechanical foot and lower limb dysfunctions.
Common Conditions Treated
Flat Feet
Plantar Fasciitis
Heel Pain
Shin Splints
Knee Pain
Lower Back Pain

Dry Needling
Inserting fine needles into trigger points or tight muscle bands to relieve pain and tension.
Common Conditions Treated
Myofascial Pain
Chronic Heel Pain
Muscle tightness and Spasms
Tendonitis

Footwear Assessment and Prescription
Expert analysis of your current footwear and professional recommendations tailored to your foot type and condition.
Common Conditions Treated
Foot Pain
Postural Issues
Overpronation

Diabetes Foot Risk Assessment
Comprehensive podiatry support for patients with diabetes, focusing on prevention, monitoring, and early intervention.
Diabetes Foot Risk Assessment include
Doppler Assessment
Monofilament(10g) Assessment
Tuning Fork Assessment
Pressure Plate Assessment
Early signs and symptoms of Diabetes Neuropathy Assessment
Footwear Assessment
Wound Assessment

Paediatric Podiatry
Specialised assessment and treatment for children with developmental, structural, or pain-related lower limb issues.
Common Conditions Treated
Flat Feet
Toe Walking
Sever’s Disease
In-Toeing
Out-Toeing

Corns, Callus & Wart Treatment
In-clinic care for painful or recurrent lesions affecting skin and nail integrity.
Common Conditions Treated
Corns
Calluses
Plantar Warts

Pressure Plate Analysis
High-resolution analysis of foot pressure distribution and gait dynamics using advanced technology.
Limb Asymmetry
Overloading
Balance
- Strength & Conditioning
- Thermal modalities
- Individualised Strength &
Conditioning Programmes - Performance & Sports-Specific Training
Programmes and Guidance - Pre / Post-Game Management & Guidance
- In-Season & Off-Season
Management Programme - Injury Prevention
- Rehabilitation & Return to Sport / Activity
- Pre & Post-Operative Strengthening

Strength & Conditioning
We go beyond just treating pain. We empower you with tailored Strength & Conditioning strategies to enhance performance, accelerate recovery, and build lasting resilience. Our expert physiotherapists integrate cutting-edge techniques with evidence-based programs to help you achieve your physical goals, whether on the field, at work, or in daily life.

Thermal modalities
Experience accelerated recovery and pain relief with our advanced Game Ready® system. This technology combines active compression with adjustable cold therapy to effectively reduce swelling, minimise pain, and optimise tissue healing following acute injuries or post-operative procedures. It's a key tool in speeding up your recovery process, allowing you to return to activity sooner and more comfortably.

Individualised Strength & Conditioning Programmes
Our core offering, this service designs personalised exercise programs to build foundational strength, endurance, and overall physical capacity. Whether you're recovering from an injury, managing a chronic condition, or simply aiming for better general fitness, we'll identify your unique needs and create a progressive plan to improve muscle function, stability, and movement efficiency for all aspects of your life.

Performance & Sports-Specific
Training Programmes and Guidance
Elevate your athletic potential with training programs meticulously tailored to the demands of your specific sport or activity. Beyond general fitness, we focus on developing the power, speed, agility, and endurance required for your performance goals. Our guidance integrates advanced exercise techniques with biomechanical analysis to optimise your movement, maximise performance, and reduce sport-specific injury risks.

Pre / Post-Game Management & Guidance
Support your body before and after competition with our specialised management strategies. Pre-game preparation focuses on optimising mobility, activating key muscles, and preventing acute injuries. Post-game management aims to accelerate recovery, reduce muscle soreness, and address any immediate concerns, ensuring you're ready for your next training session or competition. This service is designed to keep you performing consistently at your best.

In-Season & Off-Season Management Programme
For athletes, year-round strategic planning is crucial. Our In-Season Programme focuses on maintaining peak performance, managing fatigue, and preventing injuries during competitive periods, allowing you to stay on the field. The Off-Season Programme is designed for structured development, building strength, power, and addressing long-term weaknesses, setting the foundation for a stronger, more resilient next season. This holistic approach optimises your entire athletic year.

Injury Prevention
Proactive care is paramount. Our Injury Prevention service identifies your individual risk factors for common injuries through comprehensive screening and movement analysis. We then create targeted exercise programs to address muscle imbalances, mobility restrictions, and suboptimal movement patterns. By building your body's resilience and enhancing your protective mechanisms, we help you stay ahead of injuries and maintain consistent participation in your activities.

Rehabilitation & Return to Sport / Activity
This service bridges the gap between injury recovery and full, confident participation. Following an injury or surgery, we guide you through a structured, progressive rehabilitation program, focusing on restoring strength, power, agility, and sport-specific movements. Our aim is to ensure your body is fully prepared for the demands of your chosen sport or activity, minimising the risk of re-injury and getting you back stronger than before.

Pre & Post-Operative Strengthening
Optimise your surgical journey with our specialised programs. Pre-operative (Prehab) strengthening prepares your body for surgery by maximising existing strength, flexibility, and muscle control, which can significantly accelerate your post-operative recovery. Following surgery, our Post-operative strengthening provides carefully graded exercises and expert guidance to help you safely regain full strength, range of motion, and function, ensuring the best possible outcome from your procedure.
- Clinical Pilates

Clinical Pilates
Clinical Pilates is a form of therapeutic exercise developed by physiotherapists, designed to adapt traditional Pilates principles to treat injuries, improve movement control, and prevent the recurrence of pain or dysfunction. It is a personalised, evidence-based programme tailored to each client’s medical and physical needs.
Improve core stability and muscle control
Reduce pain (especially back, neck, and pelvic pain)
Enhance posture, alignment, and movement patterns
Support rehabilitation after surgery or injury
Prevent recurrence of injury
Improve balance, flexibility, and coordination
- Sports / Remedial Massage

Sports / Remedial Massage
Sports and remedial massage is a targeted therapeutic treatment that focuses on assessing and treating musculoskeletal pain, injuries, and dysfunction. Unlike relaxation massage, it uses a range of deeper techniques, including trigger point therapy, myofascial release, deep tissue massage, and stretching. Aims to identify and alleviate specific areas of tension, scar tissue, and adhesions within muscles, tendons, and ligaments.
Whether you're an athlete seeking to enhance performance, speed up recovery, and prevent injuries, or someone experiencing chronic muscle tension, posture-related pain (e.g., from desk work), or discomfort after an injury, this treatment can help. It promotes improved circulation, reduces muscle soreness, increases flexibility, and assists in the body's natural healing process, helping you move more freely and comfortably.
- Custom Made Orthotics
- Precision-Guided Design
- 3D / Heat-Moulding Technique
- Innovative Multi-Material Combinations
- Sport-Specific Performance Support

Custom Made Orthotics
1. Everyone’s feet are different
No two feet are the same — differences in arch height, foot shape, and walking patterns mean that off-the-shelf insoles often can’t provide the support your body truly needs.
2. They address the root cause of pain and misalignment
Custom orthotics help correct foot posture and alignment, reducing stress on the ankles, knees, hips, and lower back.
They are especially effective for
Plantar fasciitis
Flat feet or high arches
Knee pain
Ankle instability or poor gait
Preventing sports injuries
3. They improve comfort in both daily life and rehab
Whether you're recovering from injury, on your feet all day, or playing sports, orthotics provide targeted support to reduce fatigue and discomfort — helping you move better, longer.
4. They’re adjustable and long-term
Unlike standard insoles, our heat-mouldable, customisable orthotics can be adjusted over time to suit changes in your condition or lifestyle — making them ideal for long-term care and prevention.

Precision-Guided Design
Using Healsy’s advanced pressure-mapping system, we analyse plantar pressure distribution with exceptional accuracy. This includes digital assessment of weight loading during gait, arch height, and left–right balance to create truly personalised solutions.

3D / Heat-Moulding Technique
Flat-shaped insoles are custom-moulded using heat-forming technology to fit the unique shape of each foot. They respond flexibly to the structure and movement of the foot.

Innovative Multi-Material Combinations
With over 60 high-performance materials and 30,000+ layer combinations, Healsy orthotics are engineered to fit your lifestyle and condition. Each pair is uniquely designed to match your foot shape, movement patterns, and daily demands.

Sport-Specific Performance Support
Want to perform better in rugby, golf, basketball, football, running, or hiking? Healsy orthotics are tailored to suit the specific movements and load demands of each sport. They reduce foot fatigue and improve biomechanical efficiency — helping you move stronger and longer.
- Taping / AirCast Boots / Bracing


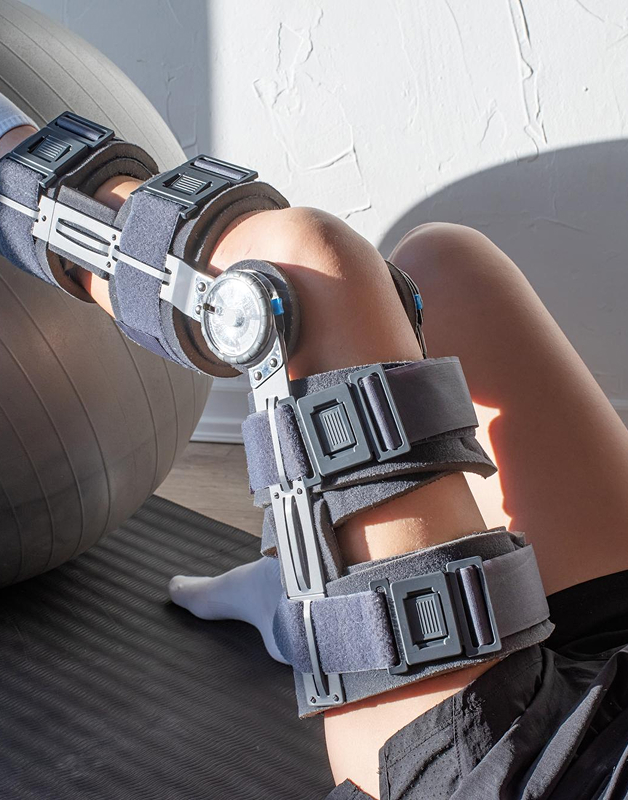
Taping / AirCast Boots / Bracing
Our clinic provides a comprehensive range of biomechanical support solutions including therapeutic taping, Aircast walking boots, and custom bracing. These interventions are designed to stabilise injured joints, protect healing tissues, offload stress from affected areas, and improve functional movement during recovery. Taping techniques, such as rigid sports taping and kinesiology taping, are used to reduce pain, support posture, and enhance proprioception. Aircast boots are ideal for managing fractures, post-operative care, and soft tissue injuries, while our selection of braces—ranging from off-the-shelf to custom-fit—address specific conditions such as ligament instability, tendon injuries, and joint degeneration. Our clinicians conduct detailed assessments to ensure the appropriate device is prescribed and fitted to support optimal healing and safe return to activity.
- EMS / ESWT / High Power Laser



Electrical muscle stimulation (EMS),
Extracorporeal Shockwave Therapy (ESWT),
High Power Laser
We offer advanced, evidence-based therapeutic modalities that promote tissue regeneration, alleviate pain, and restore function. Electrical Muscle Stimulation (EMS) is utilised to activate weakened muscles, improve circulation, and support neuromuscular re-education—particularly beneficial in post-surgical or neurological rehabilitation. Extracorporeal Shockwave Therapy (ESWT) is a non-invasive treatment that delivers acoustic pressure waves to target chronic tendinopathies, calcific deposits, and myofascial pain, stimulating the body’s natural healing response and improving blood flow. High Power Laser Therapy is used to deliver deep-penetrating photonic energy that reduces inflammation, accelerates cellular repair, and relieves pain in acute and chronic musculoskeletal conditions. These technologies are applied as part of a personalised treatment plan by experienced practitioners to maximise therapeutic outcomes and enhance long-term recovery.
- NDIS / Workcover / DVA / CTP / GPCCMP

NDIS / Workcover / DVA / CTP / GPCCMP
Our clinic is an accredited and experienced provider of allied health services under the National Disability Insurance Scheme (NDIS), WorkCover, Department of Veterans' Affairs (DVA), and Compulsory Third Party (CTP) insurance programs. We are also pleased to accept referrals under the GP Chronic Condition Management Plan (GPCCMP) plan, allowing eligible patients to access Medicare rebates for physiotherapy services referred by their GP. We are committed to delivering client-centred care that aligns with all funding requirements while addressing the unique rehabilitation needs of each individual. Whether you're recovering from an injury, managing a long-term condition, requiring functional capacity support, or accessing care through a GP referral, our team provides structured, goal-oriented treatment plans tailored to promote independence, mobility, and quality of life. We collaborate closely with case managers, insurers, support coordinators, and referring GPs to ensure timely reporting, transparent communication, and continuity of care throughout your rehabilitation journey.

Privacy policy
At Healsy Physiotherapy and Podiatry Clinic
we are committed to protecting your privacy. This policy outlines how we collect, use, store, and disclose your personal information in accordance with the Australian Privacy Principles.
INFORMATION WE COLLECT
When you visit our website, interact with our staff, utilise our software, or use our products and services, we may collect the following personal information ("Personal Data")
Full name
Company name
Occupation
Email address
Phone number
Payment details
Billing address
Geographic location
IP address
Survey responses, reviews and testimonials
We may also collect information in relation to your Patients including
Names
Gender
Date of Birth
Medical Scans results
Reviews and testimonials
You can access or amend your Personal Data by logging into your account or contacting us directly.
Please note that any information you publish on our website (e.g. blog comments or testimonials) may be publicly accessible. Even if you delete this content, cached versions may still be viewable elsewhere.
USE OF YOUR INFORMATION
We use your Personal Data to
Provide and deliver our products and services
Process payments
Communicate with you
Send updates, offers, and service notifications
Gather feedback and measure customer satisfaction
Personalise your website experience
You will only receive marketing communications if you have opted in. You can unsubscribe at any time via the link in our emails or by contacting us.
Our website also uses digital identifiers such as cookies to enhance your browsing experience by
Analysing website traffic and usage
Enable social media sharing features
Provide targeted advertising through third-party platforms
Most browsers accept cookies automatically, but you can disable them via your browser settings. Doing so may limit some functionality of our website.
We may use anonymised and aggregated data (non-personally identifiable information) to
Improve our services and website functionality
Analyse customer behaviour and website usage
Serve targeted advertisements via platforms such as Google Ads and Facebook
STORAGE AND SECURITY OF DATA
We take reasonable steps to protect your Personal Data from loss, misuse, unauthorised access, or disclosure via the following protocols.
All data is stored securely on our protected servers.
Personal data stored in paper records at our company will be physically secured.
We will not record any payment information. Credit card data is encrypted during transmission and is not stored on our systems.
Personal Data may be stored or processed outside of Australia, but only in countries that provide adequate data protection.
We retain Personal Data for only as long as necessary to provide services and comply with our legal obligations.
If a data breach occurs and your information is affected, we will notify you in accordance with applicable laws.
SHARING OF YOUR INFORMATION
We do not sell, trade, or rent your Personal Data to any third party.
Your information may be shared with third parties only when necessary to
Fulfill purchases and process payments
Provide technical and marketing support
Deliver IT infrastructure and related services
Comply with legal or regulatory requirements
Protect our rights, property, or safety
Any third-party service providers we engage are required to uphold the same privacy standards outlined in this policy and are prohibited from using your data for any purpose other than providing services on our behalf.
ACCESS TO PERSONAL INFORMATION
If you ask us, we will give you access to the personal information we hold about you. We will always confirm your identity before giving access to your personal information. However, there are circumstances under Australian privacy laws where we may not give you access to the personal information we hold about you. For example, we can’t give you access if it would unreasonably affect someone else’s privacy or if giving you access poses a serious threat to someone’s life, health or safety.
LEGAL DISCLOSURES
We may disclose Personal Data if required by law or in connection with legal proceedings, regulatory investigations, or enforcement actions.
In the event of a business transfer (e.g. merger or sale), customer information may be transferred to the new owner under a confidentiality agreement.
EXTERNAL LINKS
Our website may contain links to third-party websites for your convenience. We are not responsible for the privacy practices or content of external sites. We encourage you to review their privacy policies before providing any personal information.
CHANGE IN PRIVACY POLICY
We may from time to time update our privacy policy to ensure remains current. If we decide to so, all updates will be effective immediately upon being published.
CONTACT US
If you have any queries or concerns about our privacy policy or the use of your Personal Data, please contact us at contact@heasly.com.au

